Pancreatic Neuroendocrine Tumours (pNETs): Symptoms, Scans & Treatment
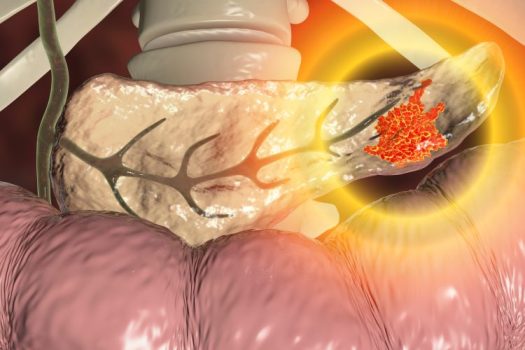
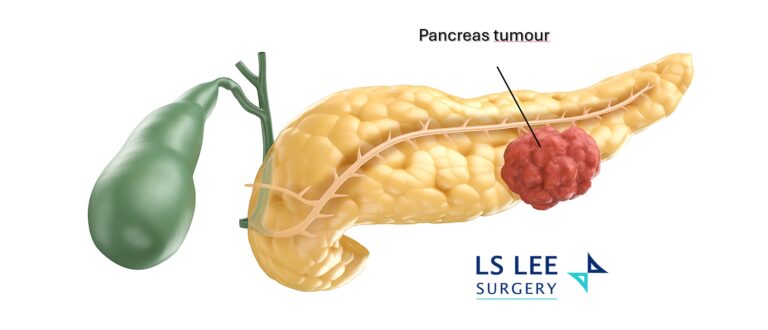
Pancreatic neuroendocrine tumours are growths that arise from the pancreas’ hormone-producing cells. Some make extra hormones (“functioning” pNETs) and cause symptoms; many do not (“non-functioning” pNETs) and are found incidentally on scans. pNETs behave differently from the more common pancreatic ductal cancer and often have different treatment options.
Key facts:
- Two broad categories: functioning (hormone-producing) vs non-functioning (most common).
- How they’re found: often incidentally on CT/MRI; functioning tumours may present earlier due to hormone effects.
- What guides treatment: size, grade/Ki-67, spread on imaging, and whether the tumour makes hormones.
- Outlook: many localised pNETs can be managed effectively with surgery; advanced cases may use targeted therapies or peptide receptor therapy (PRRT)
Common Symptoms
Most people with non-functioning pNETs have few early symptoms. Larger tumours can cause pressure-related issues.
- General (non-functioning): abdominal discomfort, unintended weight loss, jaundice (yellow eyes/skin) if the bile duct is compressed.
- Hormone-related (functioning, varies by hormones e.g. Insulinoma, Glucagonoma, Somatostatinomas, VIPoma)
- Repeated low blood sugar spells: shakiness, sweating, confusion.
- Stomach acid/ulcer symptoms: upper-abdominal pain, heartburn, nausea.
- Flushing or frequent watery diarrhoea.
If you’ve had unexplained low sugars, stubborn ulcers, or ongoing diarrhoea, a review is sensible.
Understanding your Scan Report (CT, MRI, DOTATATE PET/CT)
Reports may mention:
- “Enhancing pancreatic lesion/nodule” – how the tumour takes up contrast.
- “Well-differentiated / Grade 1–3” – how fast cells look like they can grow (often linked to Ki-67).
- “Somatostatin receptor uptake” – seen on Ga-68 DOTATATE PET/CT; helps confirm a pNET and guide PRRT.
Bring your images (not just the report) if you can—specialists often re-review the actual scans for nuance.
When to See a Specialist (Good Rules of Thumb)
- Pancreatic lesion seen on any scan
- Positive DOTATATE PET/CT or unclear CT/MRI findings.
- Symptoms suggesting hormone excess (e.g., hypoglycaemia, flushing, watery diarrhoea).
- Any uncertainty in the radiology wording—get a clear plan.
Treatment Options (Matched to Stage & Function)
Management is individualised after reviewing your scans, blood tests, and overall health.
- Surgery: Whipple (head) or distal pancreatectomy (body/tail); open, laparoscopic, or robotic—case dependent.
- Somatostatin analogues: control hormone-related symptoms and may slow growth.
- Targeted therapy: selected medicines that slow tumour growth in advanced disease.
- Peptide Receptor Radionuclide Therapy (PRRT): for tumours with somatostatin receptor uptake.
- Chemotherapy: considered for higher-grade or progressive tumours.
- Active surveillance: possible for small, low-grade, non-functioning pNETs with structured imaging follow-up.
What to Prepare for your Appointment
- CT/MRI images (USB/cloud link) and report
- Any Ga-68 DOTATATE PET/CT images
- Recent blood tests (glucose, hormones if done)
- Medication list and allergies
Dr Lee Lip Seng is an HPB (liver, pancreas and bile duct) surgeon who treats pancreatic tumours with minimally invasive approaches. When suitable, he offers laparoscopic and robotic surgery. He delivers coordinated, team-based care and sets out clear follow-up schedules and personalised treatment plans.
FAQs
Is every pNET cancer?
Many pNETs are well-differentiated and can be slow-growing. “Cancer” usually refers to the potential to spread; your tumour’s grade, size, and scans guide risk and treatment.
How are pNETs different from the usual pancreatic cancer?
They start from different cells, behave differently, and are staged/treated differently. Some pNETs grow slowly and respond to medicines that target hormone receptors.
What size is concerning?
Size is one factor. >1–2 cm, growth over time, higher Ki-67, lymph nodes, or spread on imaging raise concern and may push toward treatment.
Which scans are best?
Contrast CT or MRI define size and location. Ga-68 DOTATATE PET/CT checks for somatostatin receptors and helps decide on PRRT. Endoscopic ultrasound (EUS) may help biopsy small lesions.
Do all pNETs need surgery?
Not always. Small, low-grade, non-functioning pNETs might be watched with close imaging; others do better with surgery or systemic therapy. The decision is individual.