Pancreatic Cystic Neoplasms (PCN): Symptoms, Diagnosis & Treatment
Quick Summary
- Pancreatic cystic neoplasms (PCN) are fluid-filled growths in the pancreas.
- Types include IPMN, MCN, and SCN; IPMN/MCN may become cancerous, while SCN is usually benign.
- Many cysts are found incidentally on scans and cause no symptoms.
- Diagnosis may involve CT/MRI/MRCP and endoscopic ultrasound (EUS); sometimes a biopsy is performed.
- Treatment ranges from active surveillance to surgery (e.g., Whipple procedure or distal pancreatectomy), depending on size, appearance, location, and risk features.
- Speak with a pancreatic specialist to design an individualised plan.
A pancreatic cystic neoplasm is a fluid-filled growth in the pancreas. Most are harmless, but some—especially IPMN and MCN—can turn cancerous. Doctors assess risk using scans and sometimes EUS; low risk cysts are monitored, while high risk ones may need surgical removal.
What is a Pancreatic Cystic Neoplasm?
Pancreatic cystic neoplasms (PCNs) are a group of cysts originating from the pancreas. The main types are:
- Intraductal papillary mucinous neoplasms (IPMN): Can involve the main pancreatic duct or its branches. Some carry a risk of malignant transformation.
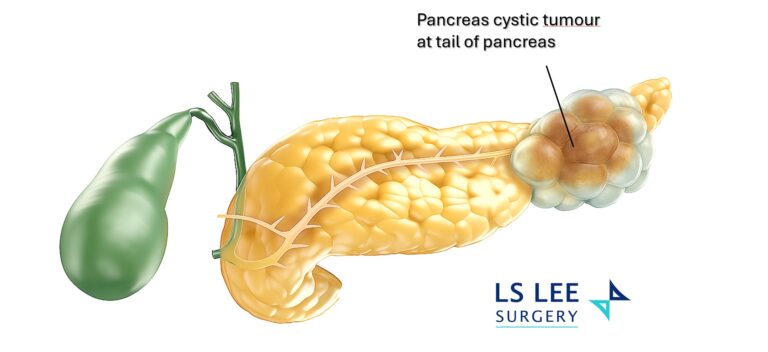
- Mucinous cystic neoplasms (MCN): Typically occur in the pancreatic body/tail and have malignant potential.
- Serous cystic neoplasms (SCN): Generally benign and often require no treatment unless symptomatic or very large.
- Other rarer cysts can occur and are assessed on a case by case basis.
Causes & Risk Factors
For many people, the cause is unknown. Less commonly, cysts are associated with underlying conditions (e.g., polycystic kidney disease) or may develop after abdominal injury.
Common Symptoms
Most PCNs are asymptomatic and found incidentally during imaging for other reasons. When present, symptoms may include:
- Vague upper abdominal discomfort
- Nausea or early fullness
- Jaundice (yellowing of skin/eyes)
- Unexplained weight loss or pancreatitis episodes
How are Pancreatic Cysts Diagnosed?
Your doctor may recommend one or more of the following:
- CT scan or MRI/MRCP: Defines the cyst’s size, location and relation to the pancreatic ducts.
- Endoscopic ultrasound (EUS): A thin scope with an ultrasound probe provides closeup images; fine-needle biopsy may be taken to analyse cells and fluid.
- Risk stratification: Features such as size, growth rate, mural nodules (internal lumps), and main duct involvement help determine if surveillance or surgery is advisable.
Treatment: Monitor or Operate?
Management depends on cyst type, size, appearance, duct involvement, symptoms, and your overall health.
Active Surveillance
Low risk cysts are often monitored with periodic imaging (e.g., MRI/EUS) to track changes over time.
Surgery
Surgery is considered when risk of cancer is higher, the cyst is symptomatic, or it shows concerning features.
- Whipple procedure (pancreaticoduodenectomy): For cysts in the head of the pancreas.
- Distal pancreatectomy: For cysts in the body/tail of the pancreas.
- Where suitable, both can be performed using minimally invasive techniques (laparoscopic or robotic) to potentially reduce pain, hospital stay and recovery time.
Your surgeon will discuss the benefits, risks and expected recovery, including whether to remove the spleen during distal pancreatectomy and the need for long term follow up.
When should I see a Specialist?
Book a consultation if you have:
- A newly discovered pancreatic cyst on imaging
- Symptoms such as jaundice, recurrent pancreatitis, or unexplained weight loss
- A cyst that is growing or has internal nodules
- When your cancer marker CA 19-9 is raised
Dr Lee Lip Seng is an HPB (liver, pancreas and bile duct) surgeon who treats pancreatic tumours with minimally invasive approaches. When suitable, he offers laparoscopic and robotic surgery. Working closely with gastroenterologists, radiologists and oncologists, he delivers coordinated, team-based care and sets out clear follow-up schedules and personalised treatment plans.
FAQs About Pancreatic Cystic Neoplasms
Are all pancreatic cysts cancerous?
No. Many cysts are benign. SCN is usually harmless; IPMN and MCN can carry a risk of cancer depending on their features.
How often should cysts be monitored?
Your schedule depends on the cyst’s type, size and appearance. Your specialist will tailor an interval (for example, every 6–12 months initially).
Is biopsy always necessary?
Not always. EUS guided fine-needle biopsy is used when the diagnosis is uncertain or when results would change management.
What are “worrisome features”?
Larger size, mural nodules, main duct dilation, or rapid growth may increase risk and prompt consideration for surgery.
Can cysts come back after surgery?
Depending on the type and whether the main duct is involved, ongoing follow up may be recommended to monitor for new changes.
What’s recovery like after minimally invasive surgery?
Many patients experience smaller incisions, earlier mobilisation, and a shorter hospital stay compared with open surgery, though recovery varies.
Do lifestyle changes help?
Healthy habits (balanced diet, avoid smoking, moderate alcohol) support overall pancreatic health and recovery, but they don’t eliminate existing cysts.