Minimally Invasive Pancreatectomy
Laparoscopy and robot-assisted surgery are two minimally invasive techniques that can be used to perform pancreatectomy, which is the surgical removal of all or part of the pancreas. These techniques offer several advantages over traditional open surgery, including less blood loss, shorter hospital stays, faster recovery times, and reduced postoperative pain.
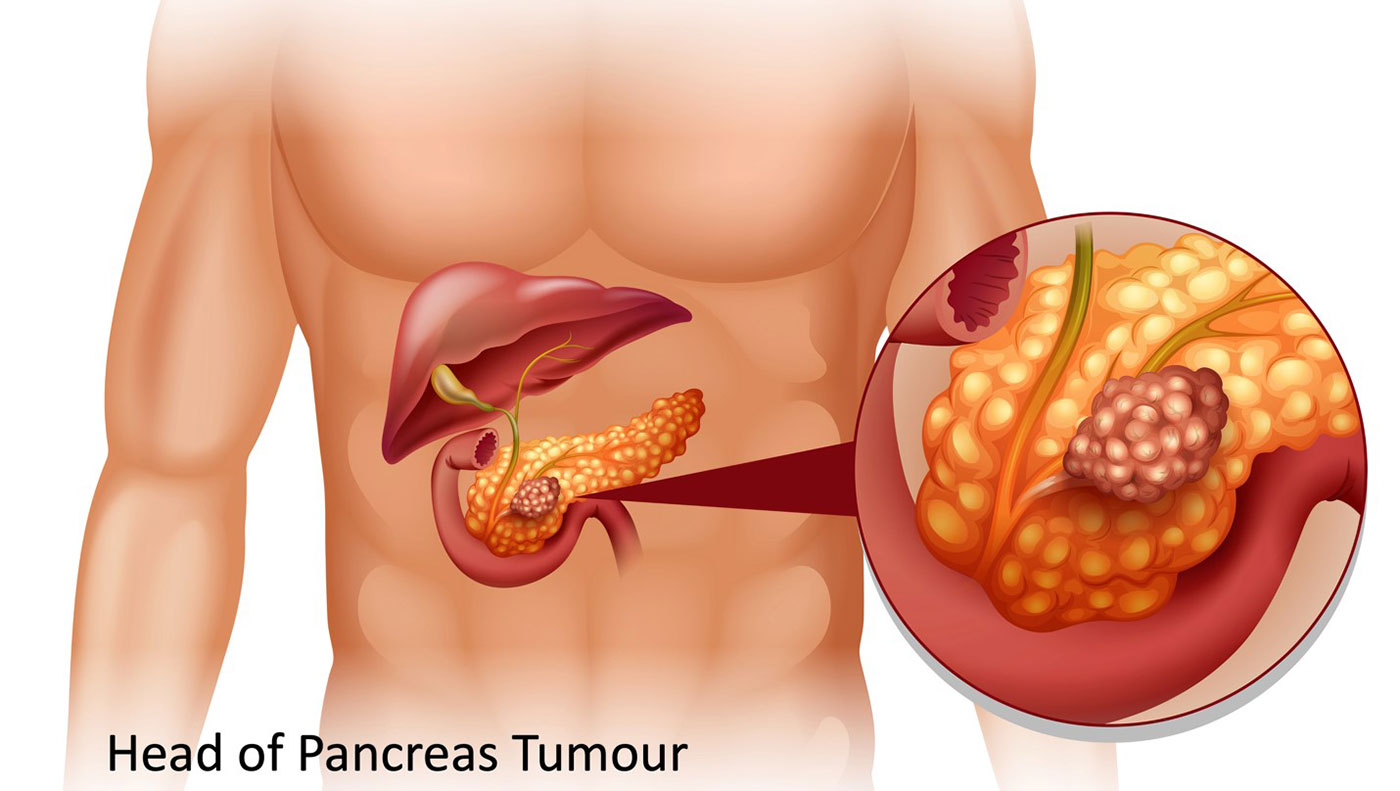
Indications for laparoscopic or robot-assisted pancreatectomy include benign or malignant tumours of the pancreas, chronic pancreatitis, and other conditions that require surgical intervention. In general, these techniques are most suitable for patients with smaller tumours or lesions that are located away from major blood vessels or other vital structures.
During laparoscopic pancreatectomy, several small incisions are made in the abdomen, through which a laparoscope and other specialized instruments are inserted. The laparoscope is a thin, flexible tube with a camera and light source that allows the surgeon to see inside the abdomen and operate with precision.
Robot-assisted pancreatectomy, on the other hand, uses a robotic system that is controlled by the surgeon. The robotic system consists of several arms that hold surgical instruments and a camera. The surgeon sits at a console and manipulates the robotic arms, which provide enhanced dexterity and range of motion compared to traditional laparoscopic instruments.

Both laparoscopic and robot-assisted pancreatectomy offer several benefits over open surgery. One of the biggest advantages is reduced blood loss, which can result in a decreased need for blood transfusions. Additionally, patients who undergo these techniques typically have shorter hospital stays, faster recovery times, and less postoperative pain. Both techniques are also associated with a lower incidence of complications such as wound infections. However, patients with advanced cancer or large tumors may not be good candidates for these techniques.
When comparing laparoscopic or robot-assisted pancreatectomy to open surgery, several studies have demonstrated that minimally invasive techniques result in a shorter hospital stay, less postoperative pain, and a faster return to normal activities. Additionally, these techniques have been associated with a lower incidence of complications such as pancreatic fistula and wound infections.
In summary, laparoscopic and robot-assisted pancreatectomy are viable options for patients who require pancreatectomy. These techniques offer several advantages over open surgery, including reduced blood loss, shorter hospital stays, faster recovery times, and less postoperative pain. However, the decision to undergo laparoscopic or robot-assisted pancreatectomy versus open surgery should be based on individual patient and tumour characteristics, as well as surgeon experience and preference. It’s important to discuss the potential risks and benefits of each approach with your surgeon to determine the best option for your specific case.