Liver Cancer Treatment in Singapore
Liver cancer occurs when abnormal (malignant) cells grow in the liver. It may be:
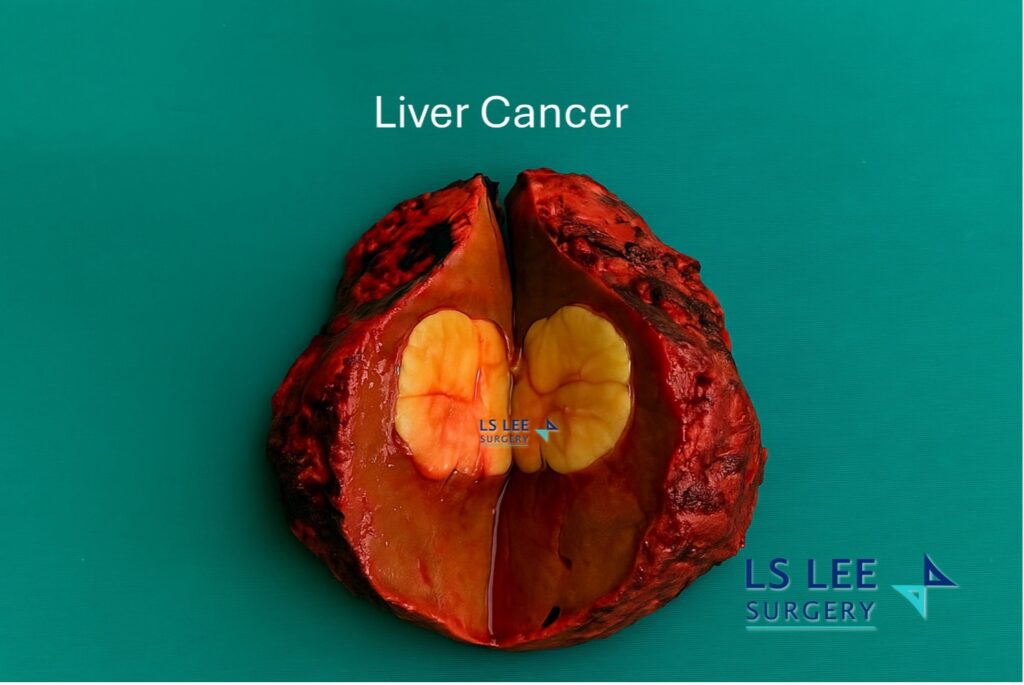
- Primary liver cancer – begins in the liver, most commonly hepatocellular carcinoma (HCC) or intrahepatic cholangiocarcinoma.
- Secondary (metastatic) liver cancer – spreads to the liver from another organ.
Early detection can widen treatment options. This page provides general information and does not replace medical advice.
Symptoms of liver cancer
Liver cancer may not cause symptoms at an early stage. Possible symptoms can include:
- A lump or fullness under the right ribcage
- Upper right abdominal or right shoulder discomfort
- Jaundice (yellowing of the skin and eyes)
- Dark urine, pale stools or itching
- Loss of appetite or unintentional weight loss
- Persistent nausea
- Fatigue or general weakness

Risk factors
Factors linked to higher risk (especially for HCC) include:
- Chronic hepatitis B or hepatitis C infection
- Cirrhosis from any cause
- Fatty liver disease (NAFLD/NASH)
- Long‑term alcohol intake
- Diabetes, obesity, or certain inherited conditions
People with these risk factors may benefit from regular liver health assessments and surveillance.
Screening and evaluation
If you are at increased risk, clinicians may recommend:
- Blood tests – liver function tests and tumour markers (e.g., AFP)
- Imaging – ultrasound, CT or MRI of the liver
- Liver biopsy – considered in selected cases when imaging is not conclusive
Not all individuals require a biopsy; the decision is based on clinical judgement and safety.
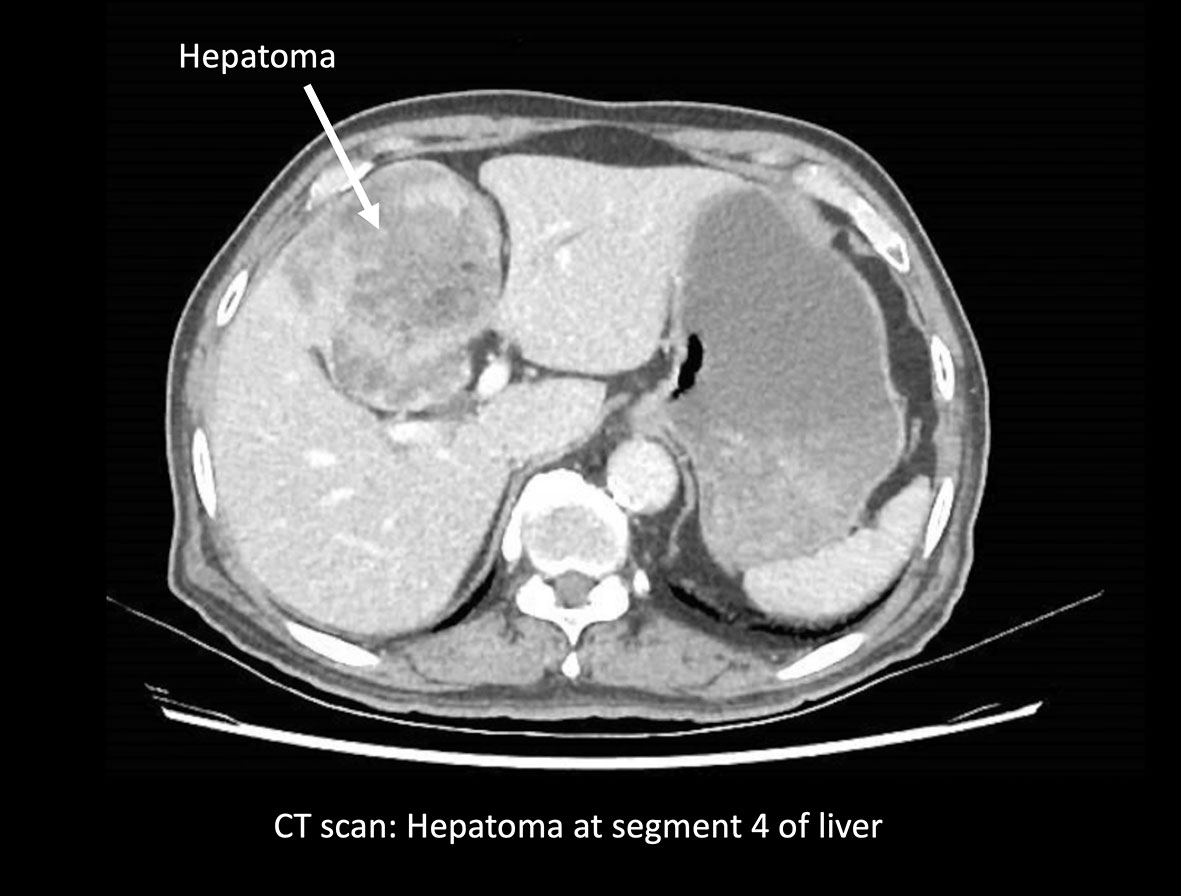
Staging and treatment planning
Staging assesses tumour size, number, vessel involvement and spread, as well as overall liver function. A multidisciplinary discussion helps match treatment to clinical needs and goals.
Treatment options
The best option depends on tumour stage, liver function and overall health. Common approaches include:
1) Surgery
When the tumour is localised and liver function is adequate, surgery may be considered.
- Liver resection – removal of the tumour with a margin of surrounding liver tissue. In suitable cases, this can be performed using minimally invasive techniques (laparoscopic or robotic‑assisted). See our page: Liver Resection with Minimally Invasive Surgery.
- Liver transplantation – considered for selected patients who meet specific criteria, often when cancer occurs alongside advanced liver disease.
2) Locoregional therapy
These therapies target the tumour within the liver and may be used when surgery is not appropriate or as part of a combined plan.
- Ablation – radiofrequency or microwave ablation uses heat to destroy tumour cells.
- Transarterial therapies – chemoembolisation (TACE) or radioembolisation deliver treatment via the tumour’s blood supply.
3) Systemic therapy
Used for advanced disease or when local therapies are not suitable.
- Targeted therapy
- Immunotherapy
- Chemotherapy (oral or intravenous)
Treatment selection is individualised and takes into account tumour characteristics, prior treatments and overall health.
Recovery and follow up
Follow up may include regular clinic visits, blood tests and imaging. Recovery time varies by treatment type and personal factors. Your healthcare team will discuss activity, work and lifestyle guidance after treatment.
Prevention and liver health
While not all liver cancers are preventable, steps that may reduce risk include:
- Hepatitis B vaccination
- Avoiding behaviours that increase the risk of hepatitis C transmission (e.g., needle sharing or unsafe tattoo/piercing practices)
- Reducing or eliminating alcohol intake
- Managing weight, diabetes and underlying liver conditions such as fatty liver disease
- Attending regular surveillance if at risk
When to seek medical advice
Consult a medical practitioner if you have persistent symptoms suggestive of liver disease or if you are at higher risk. A specialist can advise on appropriate investigations and next steps.
Look for a liver specialist:
- When you have raised cancer markers e.g. Alphafeto Protein (AFP), CA19-9 or CEA
- When there is an incidental/new liver tumour noticed on your health screening or on your follow up scans
- when the known liver tumour has changed in characteristics e.g. bigger or shapes.
Frequently asked questions (FAQ)
What are the early symptoms of liver cancer?
Many people have no early symptoms. When present, liver cancer can cause fatigue, mild abdominal discomfort or appetite changes.
Can liver cancer be cured?
Some liver cancers are potentially curable when detected early and treated appropriately. Outcomes depend on tumour stage, liver function and general health.
Is liver cancer painful?
Discomfort may occur in the upper abdomen or right shoulder region, especially in later stages.
Who is most at risk?
People with hepatitis B or C, cirrhosis, fatty liver disease or long term alcohol use have higher risk.
What treatments are available?
Depending on the clinical scenario, options may include surgery, ablation, embolisation, systemic therapy or transplantation.
Appointments
If you would like a liver specialist opinion, please contact our clinic to arrange a consultation. We will review your medical history and test results, and discuss suitable options.