Acute Pancreatitis
What is acute pancreatitis?
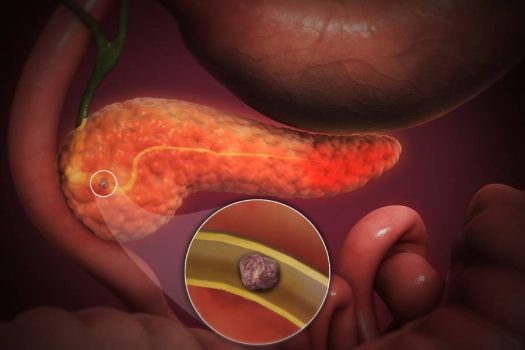
Acute pancreatitis is a condition characterized by the sudden inflammation of the pancreas, a vital organ located behind the stomach. It occurs when digestive enzymes produced by the pancreas become activated within the gland instead of the small intestine, leading to tissue damage and severe pain.
Causes of acute pancreatitis:
Pancreatitis due to gallstones is the most common cause of pancreatitis in our population in Singapore. Other causes of pancreatitis include excessive alcohol consumption, trauma, medications, high triglyceride (a type of fat) levels, and autoimmune conditions.
Presentation of acute pancreatitis:
The presentation of acute pancreatitis can vary from mild to severe and is typically characterized by the following symptoms:
- Abdominal pain: The hallmark symptom is sudden and severe pain in the upper abdomen, which may radiate to the back. The pain is often described as persistent and may worsen after eating or lying down.
- Nausea and vomiting: Many individuals with acute pancreatitis experience persistent nausea and may have episodes of vomiting.
- Fever and increased heart rate: Inflammation of the pancreas can lead to an elevated body temperature (fever) and an increased heart rate (tachycardia).
- Distended abdomen: In severe cases, the abdomen may appear swollen or distended.
- Loss of appetite: People with acute pancreatitis often have a reduced desire to eat and may experience unintended weight loss.
- Jaundice: In some cases, there may be a yellowing of the skin and eyes due to blockage of the bile duct by gallstones.
- Changes in bowel movements: Bowel movements may become oily, foul-smelling, and float due to malabsorption of fats (steatorrhea).
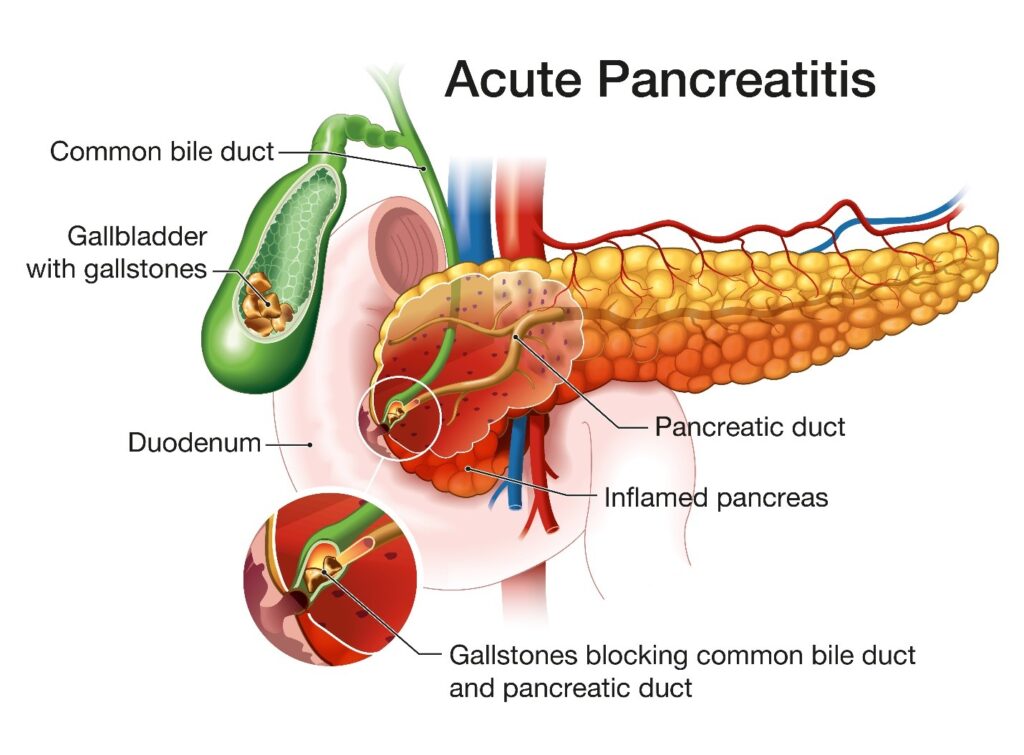
Gallstone pancreatitis:
It occurs when the gallstone in the gallbladder drops into the bile duct and blocks the common channel of the bile duct and pancreatic duct. When the pancreatic duct is obstructed, inflammation of the pancreas occurs. See diagram.
Investigation and diagnosis of pancreatitis:
The diagnosis of acute pancreatitis typically involves a combination of medical history assessment, physical examination, and various diagnostic tests. The following are common diagnostic methods used:
- Medical history and physical examination: The healthcare provider will evaluate the patient’s symptoms, medical history, and risk factors associated with pancreatitis. They will also perform a physical examination to assess for signs of abdominal tenderness, distention, and jaundice.
- Blood tests: Blood tests are crucial in diagnosing acute pancreatitis. Elevated levels of pancreatic enzymes, such as amylase and lipase, in the blood are indicative of pancreatic injury. Other blood tests include liver function tests, electrolyte levels, and markers of inflammation.
- Imaging tests: Various imaging techniques are employed to visualize the pancreas and evaluate its condition. These may include:
- Abdominal ultrasound: It can help to identify gallstones and dilatation of the bile duct (which indicate blockage of the bile duct).
- Computed tomography (CT) scan: This imaging technique provides detailed images of the pancreas, allowing for the detection of inflammation, gallstones, and complications.
- Magnetic resonance imaging (MRI): MRI scans may be used to evaluate the pancreas, especially in cases where a CT scan is inconclusive, or to assess the presence of biliary tract disease.
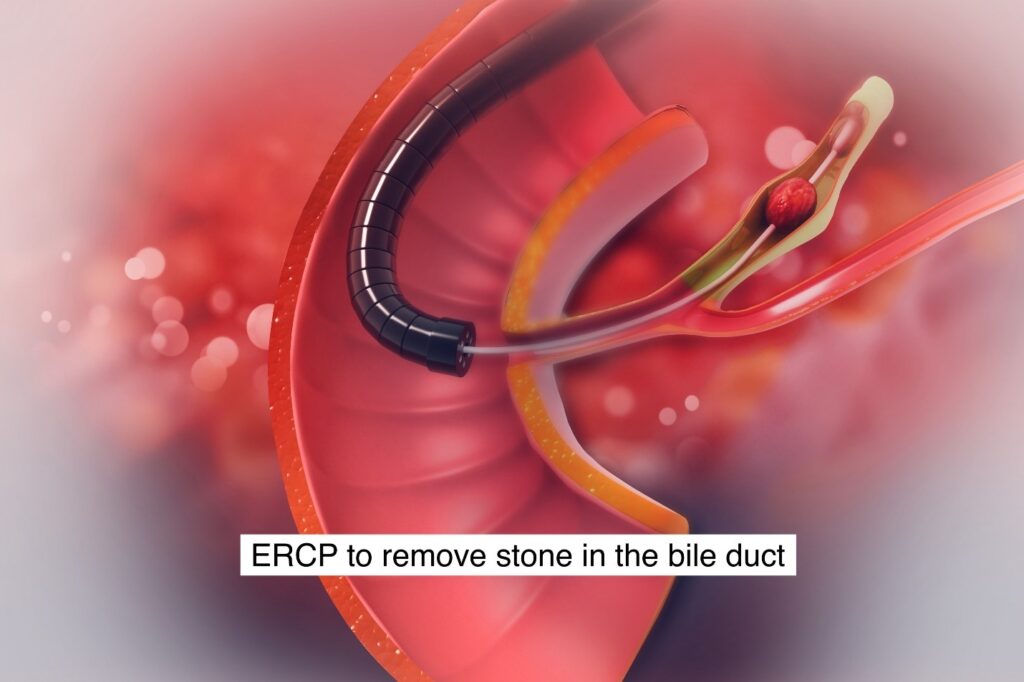
- Endoscopic ultrasound (EUS): This investigation is sometimes used when a patient is unsuitable to undergo a CT or MRI scan. It is used to look for the presence of stone in the bile duct. If EUS shows a stone in the bile duct, an ERCP can be performed at the same sitting to remove the stone in the bile duct.
Treatment:
The treatment of acute pancreatitis typically involves a combination of supportive care, pain management, addressing the underlying cause, and managing complications. The specific treatment approach may vary depending on the severity of the condition. Here are some general treatment measures:
- Hospitalization: Severe cases of acute pancreatitis often require hospitalization, especially if complications are present or if the patient is unable to tolerate oral intake.
- Fluid and electrolyte management: Intravenous (IV) fluids are administered to maintain hydration and correct electrolyte imbalances caused by vomiting and fluid loss.
- Pain management: Medications such as analgesics (pain relievers) are prescribed to alleviate abdominal pain. Stronger pain medications may be needed for severe pain.
- NPO status: Initially, the patient may be instructed to refrain from eating or drinking anything by mouth (NPO status) to allow the pancreas to rest. Nutritional support is provided intravenously or through a feeding tube if necessary.
- Addressing the underlying cause:
- Gallstone removal: If gallstones are the cause, an endoscopic procedure called endoscopic retrograde cholangiopancreatography (ERCP) may be performed to remove the gallstones from the common bile duct.
- If the gallstone pancreatitis is mild, your doctor will advise you for laparoscopic cholecystectomy to remove the gallbladder to prevent the subsequent occurrence of gallstone pancreatitis.
- Alcohol cessation: If alcohol consumption is the cause, alcohol cessation is crucial to prevent further damage to the pancreas.
- Management of complications:
- Infection control: Antibiotics may be prescribed if there is evidence of infection in the pancreas or surrounding tissues.
- Drainage: In cases where fluid collections or abscesses form, drainage procedures may be necessary to remove the accumulated fluid.
- Monitoring and supportive care:
- Close monitoring of vital signs, fluid balance, and electrolyte levels.
- Nutrition support: Once the patient can tolerate oral intake, a gradual transition to a low-fat diet is recommended.
Gallbladder removal:
Laparoscopic cholecystectomy is required to treat gallstone pancreatitis.
This is to prevent the recurrence of gallstones in the gallbladder dropping into the bile duct, causing the recurrence of pancreatitis or blockage of the bile duct, known as acute cholangitis.