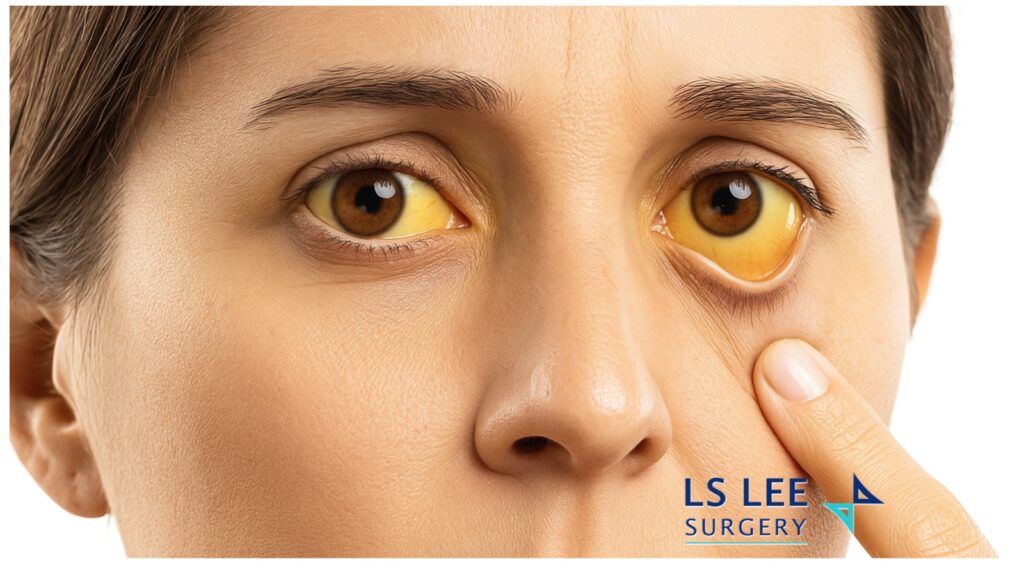
Jaundice: Causes, Symptoms, Tests & Treatment
Jaundice is yellowing of the eyes/skin from a buildup of bilirubin. It’s a sign—not a disease—and needs medical assessment. Common causes include liver inflammation, gallstones blocking the bile duct, and blood disorders. Watch for urgent red flags: fever with jaundice, severe abdominal pain, confusion, or easy bleeding—seek emergency care. Diagnosis usually starts with blood tests and an ultrasound; treatment depends on the cause (e.g., antibiotics and drainage for infection, ERCP for stones, specialist care for liver disease or cancer). If you notice yellow eyes or dark urine with pale stools, book a prompt review with a gastroenterologist/hepatologist or HPB surgeon.
What is Jaundice?
Bilirubin travels in the blood bound to albumin, then the liver processes (“conjugates”) it so it can be removed in bile. If production is too high, the liver is inflamed or not working well, or the bile ducts are blocked, bilirubin rises and the skin/eyes look yellow. The sclera often turns yellow before the skin, so it’s noticed earlier.
Common Signs & Symptoms
- Yellowing of eyes and/or skin
- Dark urine, pale or clay-coloured stools
- Itching
- Fatigue, nausea, flu-like symptoms
- Fever, chills, or abdominal pain (can signal infection)
Urgent warning signs — seek emergency care: fever with jaundice, confusion or drowsiness, severe abdominal pain, persistent vomiting, or bleeding/bruising.
What causes Jaundice? (Simple Framework)
Doctors group causes into three broad categories:
1) Before the Liver (“Pre-Hepatic”)
Excess red blood cell breakdown → too much bilirubin produced.
- Inherited or chronic haemolytic anaemias: sickle cell disease, thalassaemia, spherocytosis, G6PD deficiency
- Acquired haemolysis: transfusion reactions, autoimmune haemolysis, infections, significant trauma; occasionally endurance sports (e.g., long-distance running)
2) In the Liver (“Hepatic” / “Medical” Jaundice)
The liver can’t process bilirubin normally.
- Inherited processing issues: Gilbert’s syndrome, Dubin–Johnson syndrome; rarer metabolic disorders include Wilson’s disease and haemochromatosis
- Liver inflammation or injury: viral hepatitis (A, B, C), alcohol-related hepatitis, medication/toxin-related injury (e.g., paracetamol/acetaminophen overdose), severe infections (sepsis), malnutrition
3) After the Liver (“Post-Hepatic” / Obstructive Jaundice)
The bile duct is blocked so bile can’t drain.
- Benign (non-cancer) causes:
- Gallstones in the bile duct (choledocholithiasis), sometimes with infection (cholangitis)
- Mirizzi syndrome (stone compressing the bile duct)
- Bile duct/choledochal cysts
- Pancreatitis causing scarring/stricture
- Parasitic infections (varies by region)
- Recurrent pyogenic cholangitis (intrahepatic stones)
- Malignant (cancer) causes:
- Bile duct cancers (including hilar/Klatskin tumours)
- Gallbladder cancer
- Cancer of the head of the pancreas
- Primary or secondary liver cancers
- Periampullary or duodenal cancers
How Doctors Investigate Jaundice
Finding the cause guides the treatment.
Blood Tests
- Full blood count, liver enzymes, bilirubin (direct/indirect), clotting profile
- Viral hepatitis screens; markers of haemolysis where relevant
Imaging
- Ultrasound (first-line for many patients)
- CT or MRI/MRCP for detailed anatomy
- Occasionally PET scans (for cancer cases)
Procedures (when needed)
- ERCP (endoscopic retrograde cholangiopancreatography): a camera via the mouth to the bile duct to relieve blockages (e.g., stone extraction, stent placement) and obtain samples
- PTC/PTBD (percutaneous transhepatic cholangiography/biliary drainage): drain placed through the skin and liver if endoscopic access isn’t possible
- Endoscopic or image-guided biopsy for tissue diagnosis
Treatment: Tailored to the Cause
Most patients are managed by a multidisciplinary team, which may include a physician/hepatologist, gastroenterologist, surgeon, infectious diseases specialist, medical oncologist and radiation oncologist.
If obstruction is present
- Cholangitis (infection of an obstructed bile duct) is an emergency: antibiotics + urgent drainage (ERCP stent or PTBD).
- Gallstone-related disease: laparoscopic cholecystectomy (gallbladder removal), sometimes with common bile duct exploration.
- Benign strictures (narrowing of bile duct): may need endoscopic stenting and/or surgical biliary bypass.
If liver inflammation or failure is the issue
- Treat the underlying cause (e.g., antiviral care, alcohol cessation support, medication review).
- Severe cases may need hospital care and specialist input.
If cancer is the cause
- Evaluate for spread (metastasis).
- Potentially operable: surgery aimed at clear margins and lymph-node clearance. Depending on location, operations include bile duct resection, liver resection, or Whipple’s Procedure (pancreaticoduodenectomy). Reconstruction uses a small bowel segment to restore bile flow.
- Locally advanced or metastatic: focus on systemic therapy (chemo +/- radiotherapy), stenting for jaundice relief, and symptom control (palliative care).
- Approaches (open vs minimally invasive) depend on tumour extent and patient factors.
Possible Complications of Untreated Jaundice
- Severe itching
- Poor absorption of fat-soluble vitamins
- Abnormal clotting/bleeding
- Confusion or drowsiness due to liver dysfunction (hepatic encephalopathy)
- Sepsis from cholangitis (can be life-threatening)
Prevention & Self-Care (General Guidance)
- Vaccination where appropriate (e.g., hepatitis A/B—ask your clinician)
- Use alcohol in moderation; avoid binge drinking
- Check medications and supplements with a clinician (especially paracetamol/acetaminophen doses)
- Practice safe food and water habits in areas with hepatitis risk
- Maintain a healthy weight and balanced diet
Important: Do not self-diagnose or delay care if you notice yellow eyes/skin, dark urine, or pale stools—especially with fever or pain.
FAQs
Is jaundice a disease?
No. It’s a sign that bilirubin is high. The goal is to find and treat the cause.
Is jaundice contagious?
Jaundice itself is not. Some causes (like certain viral hepatitides) can be infectious, which is why testing matters.
Can jaundice go away on its own?
Sometimes mild causes resolve, but you should still be assessed to rule out serious conditions.
What tests will I need?
Usually blood tests first, then ultrasound. Depending on results, CT/MRI, ERCP or PTBD, and sometimes biopsy.
Which specialist treats jaundice?
HPB surgeons manage surgical/obstructive causes e.g. gallstones or tumour causing blockage; oncologists are involved for cancers; Gastroenterologists/hepatologists manage medical liver causes.
Dr Lee Lip Seng is a HPB Surgeon that treat obstructive jaundice due to cancer or gallstones with minimally invasive surgery with laparoscopy or robotic surgery. He works with his multidisciplinary team to treat his patients with jaundice or cancer.