Understanding the Relationship Between Pancreatic Tumours and Jaundice
Introduction
Jaundice is a common presenting symptom among individuals diagnosed with pancreatic cancer. However, it is important to recognize that not all pancreatic tumours lead to jaundice. Several factors, particularly the anatomical location of the tumour within the pancreas, influence whether this symptom develops. Understanding the underlying mechanisms can aid in early detection and appropriate management.
Function of the Pancreas
The pancreas is a vital organ located deep within the abdomen. It serves two primary roles:
- Digestive Function: The pancreas produces digestive enzymes that assist in breaking down food within the intestines.
- Endocrine Function: It secretes hormones, such as insulin and glucagon, which regulate blood sugar levels.
Anatomy of the Pancreas
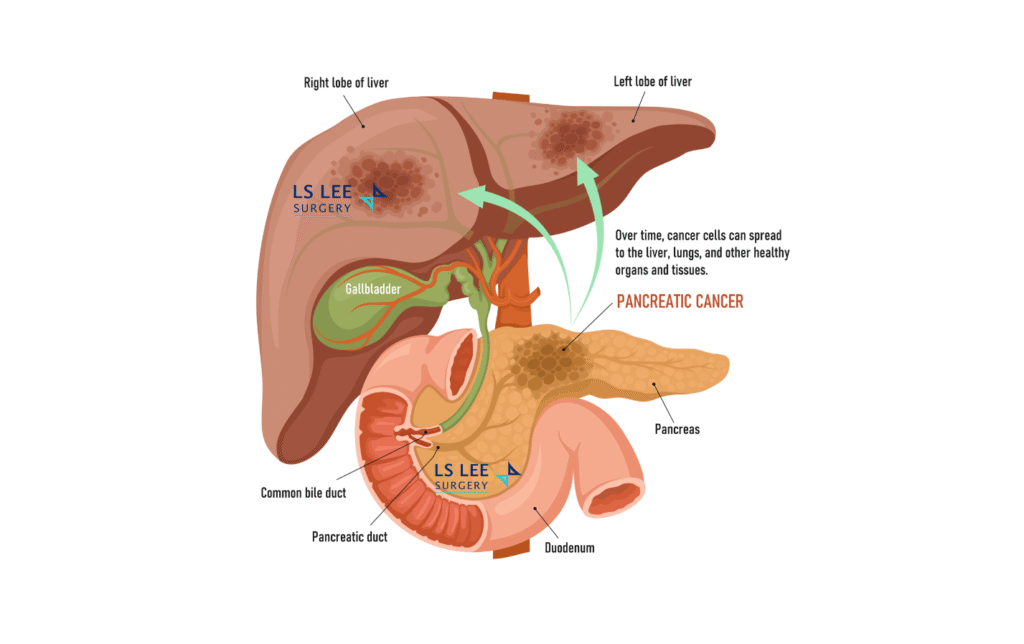
An understanding of pancreatic anatomy is essential to appreciate how tumours may or may not cause jaundice. The pancreas is an elongated organ subdivided into the head, neck, body, and tail. Running through the pancreas is the pancreatic duct, which transports digestive enzymes into the intestine. Importantly, the common bile duct, which carries bile from the liver to the intestine, passes through the head of the pancreas and merges with the pancreatic duct before entering the intestine.
Location of the Pancreas Tumour
Pancreatic tumours — including cysts, adenocarcinomas, and neuroendocrine tumours—can arise in any part of the pancreas. Jaundice typically occurs when a tumour obstructs the common bile duct, impeding the flow of bile. Patients with jaundice may notice a yellowish discoloration of the skin and eyes, dark urine, pale stools, and generalized itching.
Because the bile duct traverses the head of the pancreas, tumours located here are more likely to compress or block the duct, leading to earlier presentation with jaundice. In contrast, tumours arising in the neck, body, or tail of the pancreas are less likely to cause bile duct obstruction, often remaining asymptomatic until they reach an advanced stage. At this point, the tumour may invade adjacent structures such as blood vessels, the stomach, intestines, or lymph nodes, and potentially metastasize to distant organs like the liver and lungs. When metastatic lesions in the liver compress the intrahepatic bile ducts, jaundice can also develop, but this typically indicates advanced disease.
Conclusion
Not all pancreatic tumours result in jaundice. Tumours located at the head of the pancreas are more likely to cause early signs due to bile duct obstruction, while tumours elsewhere may progress silently. Early recognition of warning signs—such as unexplained weight loss, loss of appetite, jaundice, abdominal swelling, and abnormal liver function test or raised CA19-9 —remains critical. Timely investigation can facilitate earlier diagnosis and improved treatment outcomes for pancreatic cancers.
For specialised care under a hepatopancreatobiliary surgeon experienced in minimally invasive procedures, please contact LS Lee Surgery at 65502317.